Achieving your Financial
What’s next for Care Providers? - Your Definitive Guide to achieving your Financial Goals during COVID-19

Blog
What’s next for Care Providers? - Your Definitive Guide to achieving your Financial Goals during COVID-19

Healthcare organizations across the care continuum are making sweeping changes to suspend elective surgeries and deliver maximum support.
T he American Medical Group Association (AMGA) is taking new initiatives to expand the financial benefits by seeking further advances in Medicare reimbursements, improved flexibilities in digital health, telemedicine and remote patient monitoring capabilities —to mitigate the impact of the surging cases of the COVID-19.
The AMGA community members are witnessing huge spikes in coronavirus cases and are encouraging Congress to lend additional financial support to hospitals and practices during these testing times.
With the COVID-19 cases topping over 181,000 in just a day and the hospitalizations having hit a record high of over 69,000, AMGA has sent a letter to Congressional leaders, calling for additional support for the frontline providers. The plea included additional funding for COVID-19 Cares Provider Relief Fund and the expansion of Medicare’s Accelerated and Advance Payments (AAP) Program, among the others.
The surging pandemic, influenza and the coming winter season bring a confluence of emerging challenges that need to be quickly addressed. The health systems and medical communities are making contingency plans to postpone elective procedures and further leverage ‘hospital beyond walls’ capabilities—to mitigate the risks of further damage, according to AMGA.
Healthcare organizations across the care continuum are making sweeping changes to suspend elective surgeries and deliver maximum support.
“As of November 16, we are taking several initiatives to stall elective surgeries, that can be safely postponed to future dates. It’s critical that we take these drastic measures as part of our capacity management and resource maximization efforts—to ensure timely interventions and the best care for our patients. The available rooms will still fall short of expected care delivery if there is no nurse at the bedside, according to global healthcare leaders,” explained in the letter.
Alternatively, hospitals and practices are also rolling back elective surgeries—post the Centers for Medicare & Medicaid Services (CMS) announcement on the relaxation of non-emergent, elective medical services, as part of the three-phased approach of Opening up America Again.
These decisions underscore the significance of having a more inclusive strategy that considers clinical, operational and financial implications of the new initiatives. Consider that providers, especially small practices were facing major financial losses and even practice closures, as a result of the after-effects of COVID-19 contingency measures.
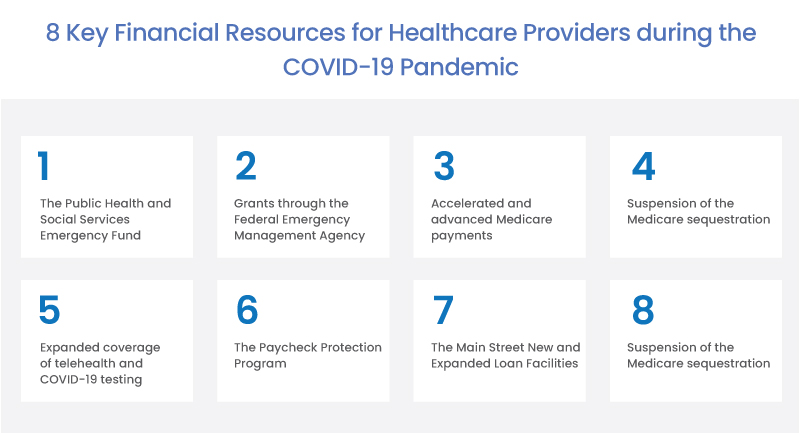
To flatten the curve, congress infused billions of dollars to support care providers through the 2T Stimulus package. However, another bill that provider communities have been looking forward to, seems to be off the radar.
Legislative actions must be taken to expand the benefits of financial aid initiatives to help providers maintain the financial viability and rise above the upcoming challenges and revenue losses. The medical communities are also calling on Congress to make significant policy changes in terms of telemedicine guidelines and telehealth reimbursements.
Since the COVID-19 outbreak, CMS has been making several announcements to relax policies and regulations regarding care providers’ financial aid, Accelerated and Advance Payment Program, telemedicine guidelines, telehealth reimbursements and regulatory protocols for remote patient monitoring among many others. CMS also understood the need for patients without smartphones to access care and created new opportunities by creating new audio codes for those patients. It’s even more crucial that Congress recognizes the significance of telehealth solutions and act quickly to lift some of the norms and restrictions that intervene in maximizing the telemedicine solution benefits.
President Joe Biden has made announcements on further supporting another COVID-19 stimulus package and has encouraged Congress to agree on the legislation to mitigate the financial implications.
Stay tuned to stay on top of the COVID-19 initiatives, innovations, policies, guidelines and the latest healthcare—you don’t want to miss!
To learn more on telemedicine reimbursements, outcome-driven patient engagement solutions or to get your free and personalized consulting and report on your medical billing strategies, talk to our team
From our humble beginnings as a healthcare start-up—to becoming a full-blown healthcare-exclusive digital transformation provider, our journey has been quite a remarkable one. Today, SolvEdge is a leading-edge Healthcare services and solutions provider—trusted by 450+ Hospitals, 3500+ Physicians and millions of patients across the globe.