Denial Management Program
7-Point Checklist to a Successful Claim Denial Management Program

Blog
7-Point Checklist to a Successful Claim Denial Management Program

The good news is that 90% of claim denials are preventable! However, the healthcare revenue cycle management is a complex framework that involves intricate processes, multiple stakeholders and hence a nuanced approach and a robust denial management program to achieve sustainable results.
Denial Management in Medical billing has witnessed a paradigm shift in the last five years, especially since 2020, when claim denials hit an all-time high! Reports indicate that over 33% of hospitals were nearing the “danger zone” with an average claim denial rate exceeding 10%. However, the good news is that 90% of claim denials are preventable! However, the healthcare revenue cycle management is a complex framework that involves intricate processes, multiple stakeholders and hence a nuanced approach and a robust denial management program to achieve sustainable results.
This blog outlines a Seven-point checklist that helps take a strategic approach to revenue cycle denial management.
Before orchestrating a denial management plan, harness the analytical capabilities to understand the past and the present denial rates to evaluate process efficiencies and determine the areas of improvement.
When the denials are not tracked, it leads to poor revenue cycle performance. This in turn results in increased denials that impact the overall revenues, cash flow and the financial health of a healthcare organization. Hospitals and medical practices need to integrate secure and highly compliant denial management tools and applications to streamline and monitor the entire process.
Stay on top of the claims denial management process by automating and streamlining workflows and getting a 360-degree view of the dashboards and frameworks for better insights on the current state of denials. Gather all the relevant details from the payors. Leverage data and analytics to derive actionable insights on the root causes and the common patterns of claim denials. This will help fix the denial challenges from the root.
Follow a stringent process to quickly address denied claims—ideally within a 24-hours timeframe. Leverage the capabilities of advanced denial automation software tools and an automated process of denial management in medical coding to accelerate the speed and improve process efficiencies
Use advanced reporting tools to provide deep insights into your operations. A comprehensive service suite that analyzes predictive payor mix data, financial benchmarking reports, utilization or denial code trends—to focus on categorizing denials that are most likely to get approved on resubmission and eliminate claims that may get denied.
Get in-depth insights on the denial management process to evaluate process efficiencies and identify areas that needs to be addressed for optimal denial management performance. Denial automation is a significant step that helps improve speed, accuracy and efficiency of the entire revenue cycle management process.
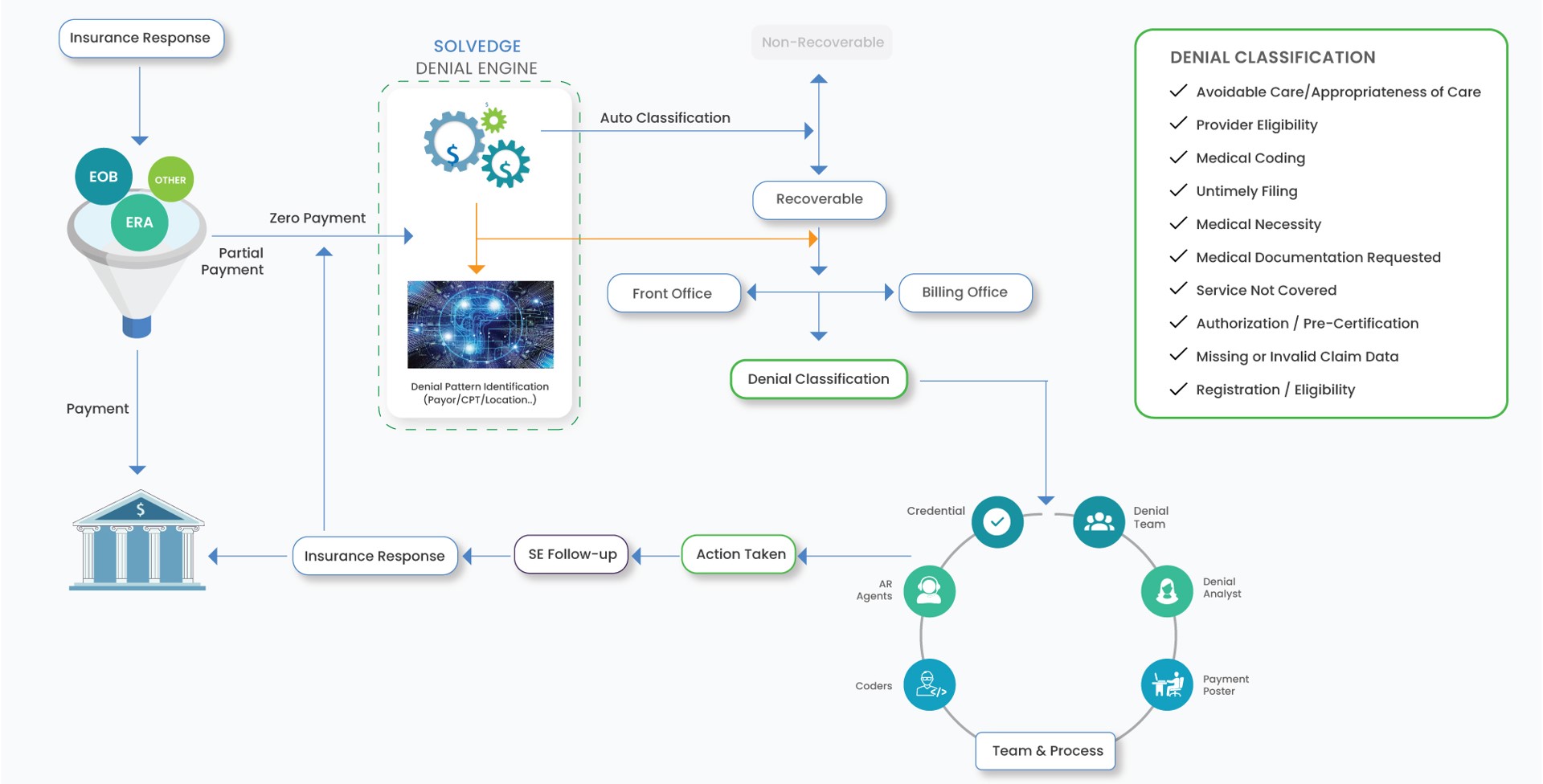
At SolvEdge, our denial management services and strategies are uniquely designed to reduce the spiking denial rates, while having a proactive approach to denial prevention. Our customized workflows help determine the root cause of denials. Once the denial patterns are identified, we create a detailed report that evaluates the recurring causes of claim denials. By leveraging these insights, we implement process improvements to reduce denials and optimize revenues.

To learn how SolvEdge’s denial management services can help reduce your claim denials and maximize your financial performance, Contact Us
From our humble beginnings as a healthcare start-up—to becoming a full-blown healthcare-exclusive digital transformation provider, our journey has been quite a remarkable one. Today, SolvEdge is a leading-edge Healthcare services and solutions provider—trusted by 450+ Hospitals, 3500+ Physicians and millions of patients across the globe.