Denial Management
Denial Management Services: It’s Time to Collect Every Dollar Due!

Blog
Denial Management Services: It’s Time to Collect Every Dollar Due!

Denial Management Services have various components of which Claim denials is one of the most frustrating challenges faced by the medical billing team and the healthcare system executives.
Denial Management Services have various components of which Claim denials is one of the most frustrating challenges faced by the medical billing team and the healthcare system executives. Claim denials have a direct negative impact on an organization’s bottom line, and claim appeals by itself is quite an exhaustive process—consuming a massive amount of time and money, even if successful.
24 hours is all it takes to
While Hospitals and Practices, need an effective denial management services strategy to rework denied claims, it’s time for care providers to shift their focus from denial management to denials prevention—to achieve sustainable results. When claims are processed without a hitch, it helps both Payers and Providers maintain a smooth and effective revenue cycle process on the whole. Denial prevention has multiple benefits for care providers helping them give transparent bills in terms of patient financial responsibilities—thereby improving patient experience and satisfaction, while improving collections.
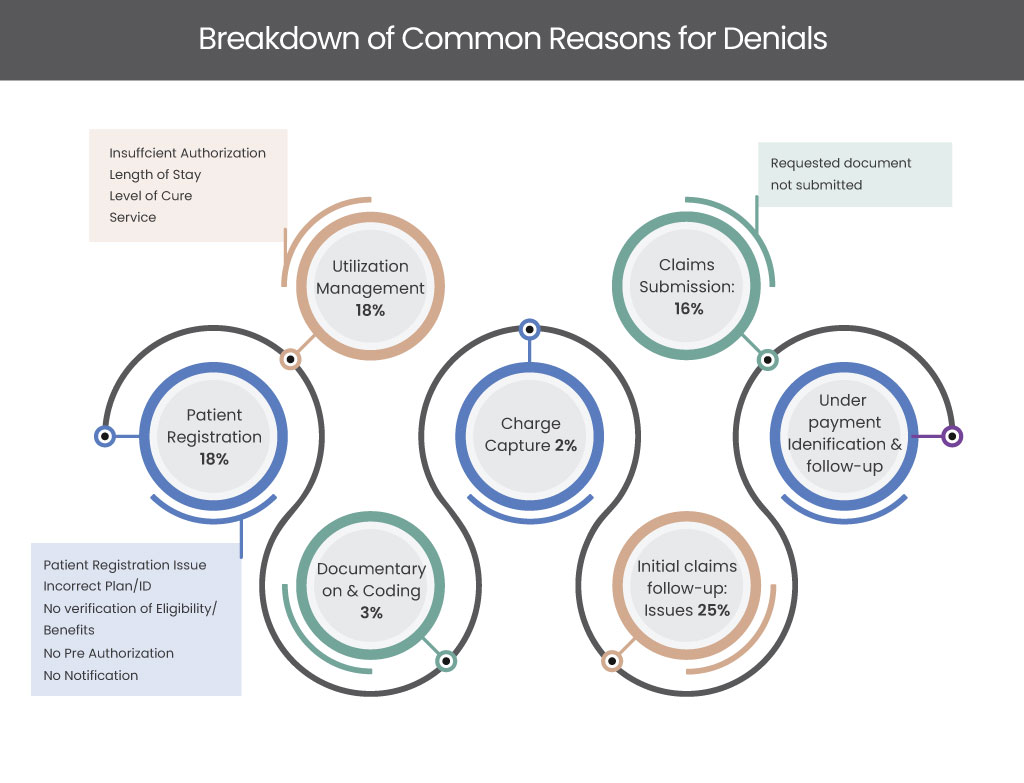
A comprehensive denial management program comprises a 360-degree approach—starting from claim documentation and submission through claim appeals if required. It includes three major components:
Data that can be deciphered and converted to actionable insights plays a significant role in the success of a revenue cycle program. Furthermore, specific data segmented as per Payer behaviors, CPT codes, Physicians, diagnosis and other customized categorizations provide actionable healthcare insights that mitigate the effects of denials—while giving a comprehensive view into denial prevention. Analytics and automation provide in-depth insights on payer behaviors, which help identify the denial patterns and mitigate the barriers to reimbursements.
The primary goal of the claim recovery process is to get fair and timely reimbursements. However, claim denials are at an all-time high! There’s been a whopping 20% increase in claim denials in the past five years. The global pandemic has only made this trend worse. The sudden spike in denials has put over 33% of Hospitals and Medical Practices in danger zone, creating enormous pressure on especially independent Practices.
The surge in claim denials has slowed down claim recovery process, as the Hospital and Practice administrative staff are overwhelmed with the spiking denial rates, that has shifted their focus away from claim appeal management. With valuable payer data in place, care providers can leverage Artificial Intelligence-powered technologies to partially automate the appeals process.
When claim denials have reached a point of escalation, it requires human intervention where the denial management service team delves into the nuances and the intricacies of the denials to get an in-depth understanding of claims management. To ensure that the escalation process is maximized, the medical billing service team needs to optimize the workflows. At SolvEdge, our denial management service team is well-equipped with an expert team of certified professionals, Doctors, PhDs, SME’s, technologists who seamlessly work together to simplify claims management
At SolvEdge, our denial management services and strategies are uniquely designed to reduce the spiking denial rates, while having a proactive approach to denial prevention. Our customized workflows help determine the root cause of denials. Once the denial patterns are identified, we create a detailed report that evaluates the recurring causes of claim denials under various categorizations like the Payer, doctor, diagnosis and CPT codes. By leveraging these insights, we implement process improvements to reduce denials and optimize revenues. SolvEdge’s uniquely designed 4Clover program for denial management is a time-tested and proven approach (with the phases—1. Analyze, 2. Strategize, 3. Discover & 4. Implement) that ensures maximized revenues and collection of every dollar due!

We don’t improve your collections as promised.
That’s how serious we are about your denials and prevention! But you “don’t have to bet us” on this. Here's how you can take the challenge yourself!
From our humble beginnings as a healthcare start-up—to becoming a full-blown healthcare-exclusive digital transformation provider, our journey has been quite a remarkable one. Today, SolvEdge is a leading-edge Healthcare services and solutions provider—trusted by 450+ Hospitals, 3500+ Physicians and millions of patients across the globe.