Claim Denials: Hospitals
33% of Hospitals in “Danger Zone” with 10% Claim Denials: Here’s How to Change the Trend

Blog
33% of Hospitals in “Danger Zone” with 10% Claim Denials: Here’s How to Change the Trend

A well-orchestrated denial management service strategy powered by insightsdriven automation technologies goes a long way in preventing claim denials, improving process efficiencies and accelerating revenue cycle performance.
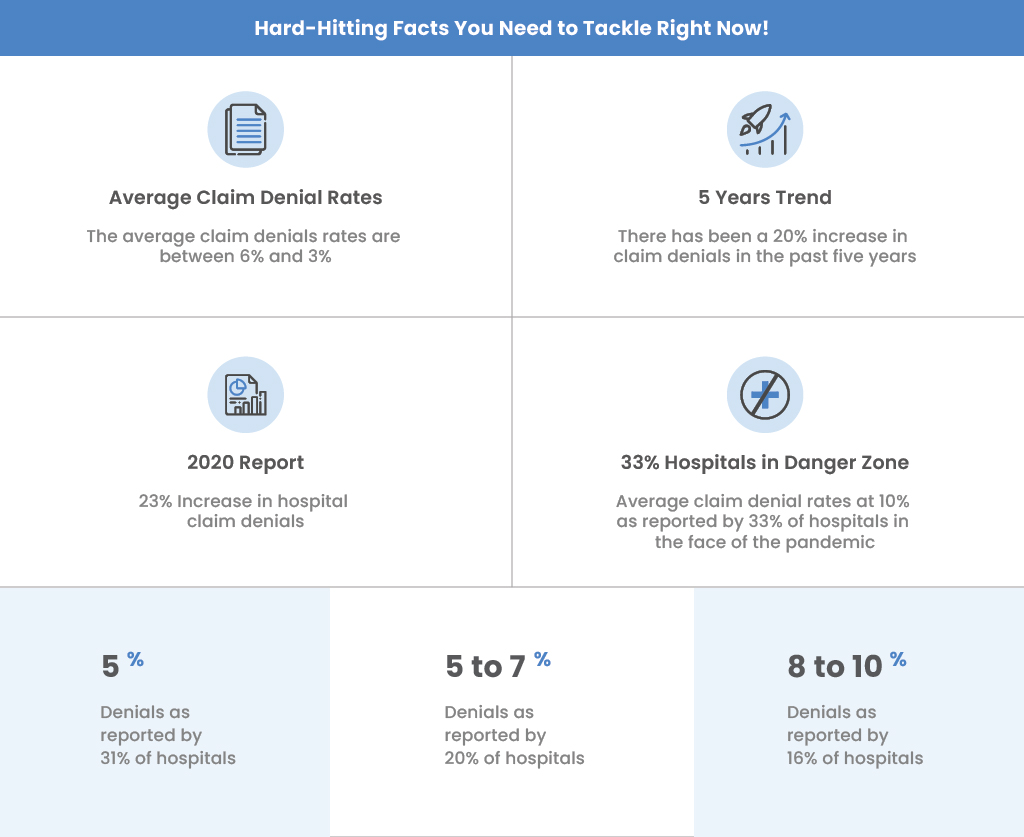
Medical billing Claim Denials among healthcare organizations are at an all-time high! While the average claim denial rates are between 6% and 13%, the COVID-19 outbreak has pushed over 30 percent of hospitals to the “danger zone” with a reported average claim denial rate of 10% or higher, in the face of the global pandemic
The Good News: 90% of Claim Denials are avoidable!
Global research on denial management has identified that 90 percent of claim denials are avoidable. A well-orchestrated denial management service strategy powered by insightsdriven automation technologies goes a long way in preventing claim denials, improving process efficiencies and accelerating revenue cycle performance.
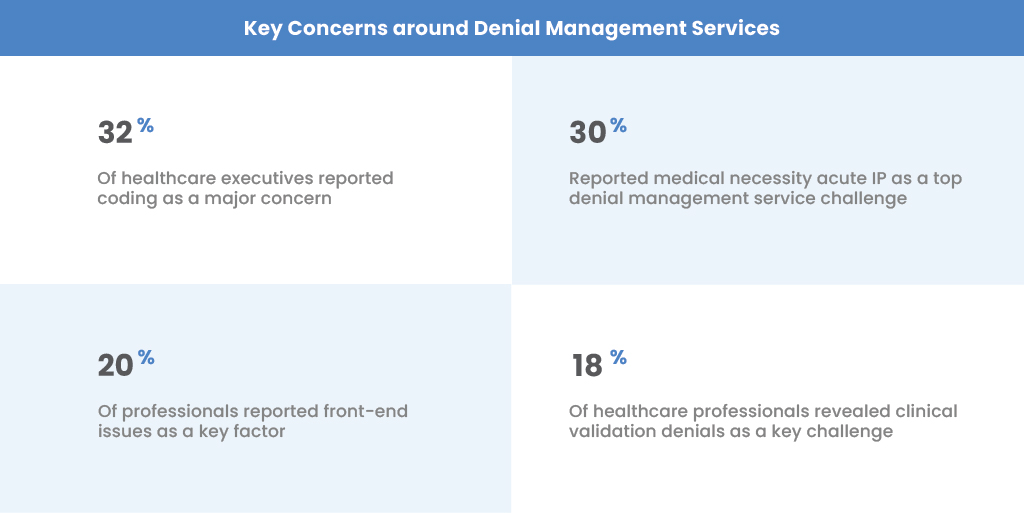
Denial management in medical billing could be seen as a backend process, but prior authorizations are primarily front-end responsibilities that need careful planning. Consider the fact that a whopping 80 percent of claim denials are attributed to prior authorization concerns.
So, how do we fix this?
Payer Policy Manager. The Payer Policy manager helps you categorize and streamline the essential prerequisites so the medical billing services team stays on top of the services that require prior authorizations, which can then be linked to the respective CPT codes.
Eligibility Verification. Your medical billing and coding services need to have the eligibility verification processes intact—to determine the need for prior authorization to be part of the workflow. Automation, driven by next-gen artificial intelligence technologies, can simplify processes, mitigate errors and significantly improve accuracies along the process.
Scheduled Services and Anticipated Services. While partial automation can enhance process efficiencies and improve financial outcomes, there are critical aspects involved in other stages that require manual intervention. One of them is to get prior authorizations by considering not just scheduled medical services and procedures but also anticipated services analyzing other possible procedures or medical services that might be required—depending on the results of the scheduled services.
Evaluating Possible Scenarios of a Claim Denial. Listing out the several possibilities of denials and carefully documenting them would help in predictive and prescriptive models of care— further facilitating the care providers with the medical necessities for the procedure.
Track and Monitor Prior Authorization Denials. It is critical that all the prior authorization denials are carefully monitored and documented to avoid confusions at later stages. Segment them into various categories based on CPT codes, Physicians and other criteria that you may find relevant and necessary. These data will drive actionable insights that proactively prevent future claim denials at large.
6 Key Strategies to Improve Denial Management Services in Healthcare Revenue Cycle
Top Ways to Improve Denial Management Process for Accelerated Revenue Cycle Performance
Automating Healthcare Revenue Cycle Management Services for Faster Reimbursements
8 Questions to Ask Before you hire a Medical Billing Company
10 Reasons to Consider Outsourcing Healthcare Revenue Cycle Management Services
To learn more about how denial management outsourcing can help drive your healthcare organization’s revenue cycle performance, talk to our team.
From our humble beginnings as a healthcare start-up—to becoming a full-blown healthcare-exclusive digital transformation provider, our journey has been quite a remarkable one. Today, SolvEdge is a leading-edge Healthcare services and solutions provider—trusted by 450+ Hospitals, 3500+ Physicians and millions of patients across the globe.