Optimizing Healthcare Insurance
Optimizing Healthcare Insurance Eligibility Verification: Getting Claims Accepted on the First Go!

Blog
Optimizing Healthcare Insurance Eligibility Verification: Getting Claims Accepted on the First Go!

In this article, we will discuss the key tactics to improve healthcare insurance eligibility and maximize your revenue cycle performance.
The current healthcare landscape is more complex—not just for healthcare providers but for patients too. Studies show that most insurance claim denials happen due to gaps in patient information like—incorrect form filling, expired health insurance policies, missing claims form, lack of pre-certification, among many others.
In this complex scenario, it is critical that care providers rethink their revenue cycle strategies to make the insurance verification process more effective. In this article, we will discuss the key tactics to improve healthcare insurance eligibility and maximize your revenue cycle performance.
Insurance eligibility verification is amongst the key processes in the overall revenue cycle management-as it has a direct impact on claim denials and payment delays. An ineffective insurance eligibility verification process affects all the aforementioned areas-disrupting reimbursements, revenues and the entire revenue cycle process.
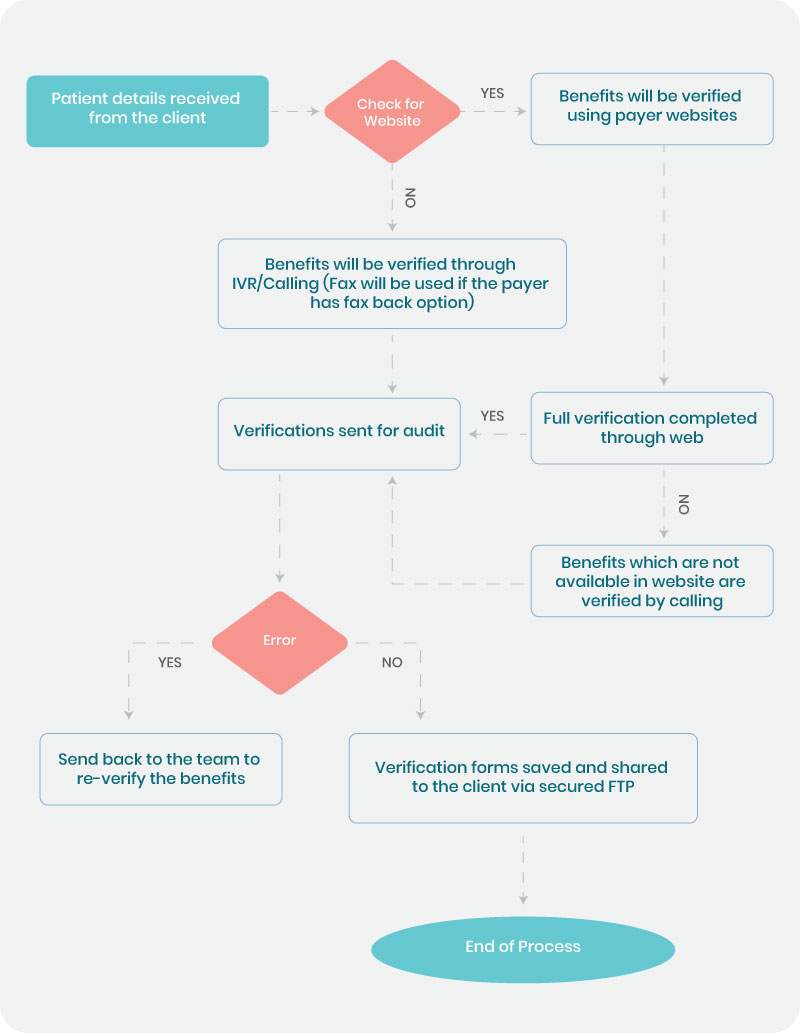
Confirming the insurance coverage facilitates claim acceptance on the first go, whereas non-verification leads to several inconveniences like decreased patient satisfaction, increased errors, claim delays and denials. A strategic and step-by-step verification process is key to reducing claim denials and A/R days.
The Centers for Medicare & Medicaid Services (CMS) report reveals that about one third of claims are rejected on the first submission, and a whopping 67 percent of physician practice revenue is lost due to billing leak. Also, studies show that ineffective insurance eligibility verification process is amongst the top five reasons for claim denials.
Two of the key reasons for claim denials include-incomplete eligibility verification forms and invalid insurance coverage under a specific plan for the patient. Sometimes the in-house staff responsible for insurance verification may be overwhelmed with high-priority tasks like-documenting patient check-in and checkout, addressing patient concerns, scheduling appointments and multiple other tasks, which may lead to manual errors. Essentially, the primary reasons for claim denials include inaccurate claim submissions and failure to update the existing insurance coverage details. This in turn leads to delayed reimbursements, reduced cash flow, increase in A/R days that affect the entire revenue cycle process.
Our Medical billing service team experts at SolvEdge recommend 6 techniques that can optimize your insurance eligibility verification process.
At SolvEdge we understand that insurance eligibility verification can make or break the overall medical billing process. Our comprehensive strategies are designed to
SolvEdge’s dedicated insurance eligibility verification team is equipped with well-trained, certified and experienced staff (5+ years of experience on an average) as we leverage cutting-edge technologies, strategic processes and industry best practices-to significantly reduce claim denials, A/R days, and ultimately optimize the revenue cycle process.
To learn more about how SolvEdge can help your organization streamline and maximize your eligibility verification process, talk to our team.
From our humble beginnings as a healthcare start-up—to becoming a full-blown healthcare-exclusive digital transformation provider, our journey has been quite a remarkable one. Today, SolvEdge is a leading-edge Healthcare services and solutions provider—trusted by 450+ Hospitals, 3500+ Physicians and millions of patients across the globe.