Orthopedic Denials
Top Ways to Streamline Coding and Denial Management Workflows in Orthopedic Billing

Blog
Top Ways to Streamline Coding and Denial Management Workflows in Orthopedic Billing

The Centers for Medicare & Medicaid Services (CMS) has clearly set policies and reimbursement rates for providers and follows the Physician Fee Schedule guidelines to streamline the billing process. Medical billing and coding for orthopedic surgeries have very similar guidelines.
The Centers for Medicare & Medicaid Services (CMS) has clearly set policies and reimbursement rates for providers and follows the Physician Fee Schedule guidelines to streamline the billing process. Medical billing and coding for orthopedic surgeries have very similar guidelines. However, the global pandemic has had adverse effects on the medical billing reimbursements for orthopedic surgeries.
For instance, consider that the federal COVID-19 relief packages could have a significant impact on the additional cuts, while leaving lower margins for small practices and physicians. While reimbursement cuts are inevitable in the current scenario, one of the major concerns is that these cuts should not limit patient access to care at the time when they need it the most.
There has been a paradigm shift in the coding and billing policies for providers including the reimbursements for orthopedic surgeries. CMS has announced various policies in 2021 under Medicare Physician Fee Schedule (MPFS) to reduce orthopedic surgical services by at least 5%. This is bound to add to the financial burdens of orthopedic hospitals and practices that are already adversely affected by the financial impact of the public health emergency.
This article focuses on the top reasons for claim denials in orthopedic billing and gamechanging strategies to improve orthopedic surgery reimbursements
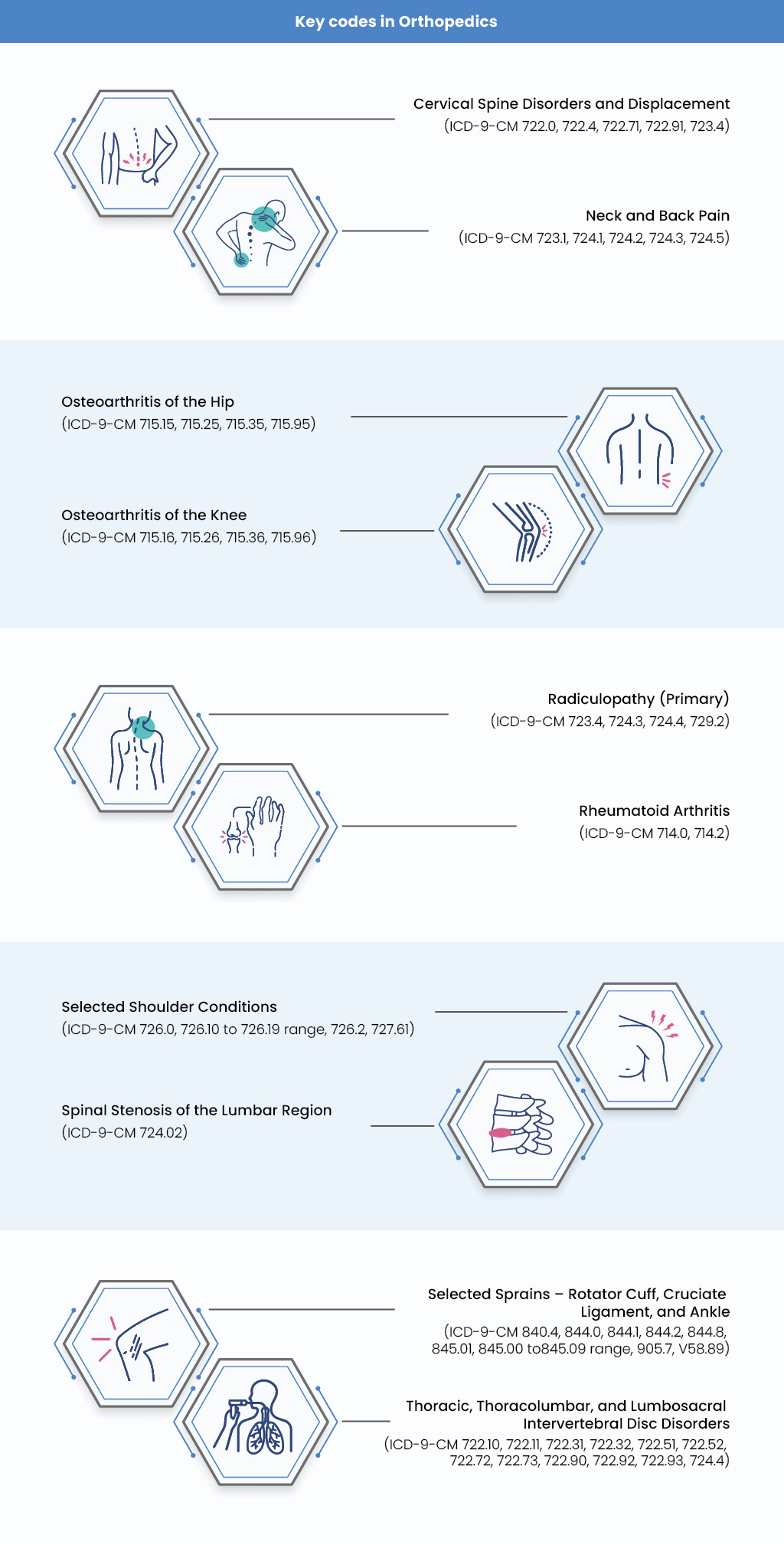
Three types of denials constitute orthopedic billing.
2021 OPPS Final Rule: Key Takeaways from the CMS Policy
Medicare Physician Fee Schedule: CMS Update
CMS Proposes to Permanently Expand Telehealth Service Benefits
CMS Interoperability and Patient Access Final Rule
Top Tactics to get Upfront Healthcare Reimbursements during COVID-19: CMS Accelerated and Advance Payment Program
$2T Stimulus: Restructuring Healthcare Ecosystem
To learn more about how your healthcare organization can prevent orthopedic denials and improve denial management services, talk to our team.
From our humble beginnings as a healthcare start-up—to becoming a full-blown healthcare-exclusive digital transformation provider, our journey has been quite a remarkable one. Today, SolvEdge is a leading-edge Healthcare services and solutions provider—trusted by 450+ Hospitals, 3500+ Physicians and millions of patients across the globe.