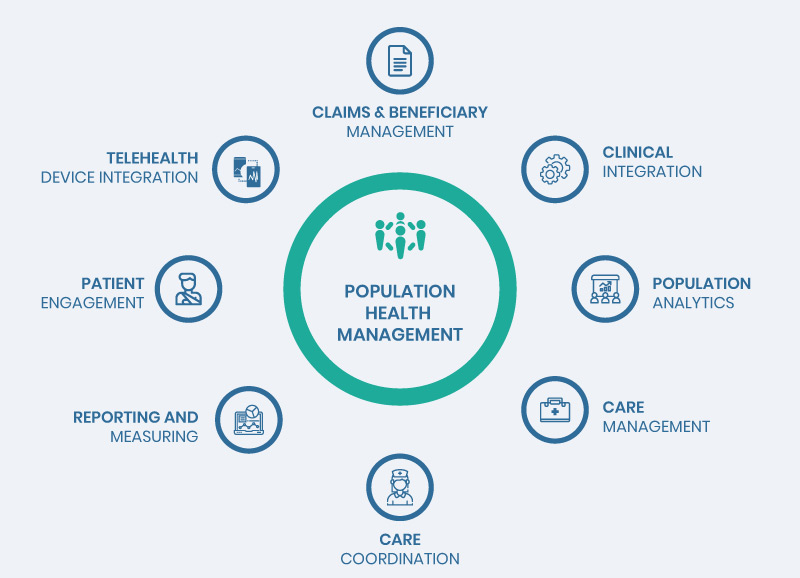
Population Health Management
Population Health Management: Shifting Towards Value-based Healthcare

Blog
Population Health Management: Shifting Towards Value-based Healthcare

Rather than focusing on smaller patient populations and samples, the industry professionals are having a broader perspective in today’s healthcare landscape, aiming to capture huge data samples and create innovations for the shifting trends from the current payment models.
T he surging demand for value-based care has led to a huge spike in the adoption of Population Health Management (PHM). The global Population Health Management market value was at $26.7 billion in 2019 and is prognosticated to grow at a CAGR of 25.6% to 166.7 billion by 2027.
Increasing rate of chronic diseases, greater adoption of healthcare technologies, need for continuous surveillance, development initiatives such as partnerships and agreements and increasing government participation, among many other factors contribute to the growth of Population Health Management.
Rather than focusing on smaller patient populations and samples, the industry professionals are having a broader perspective in today’s healthcare landscape, aiming to capture huge data samples and create innovations for the shifting trends from the current payment models.
The BIG Idea – Accelerating Success
Moving towards population level of thinking comes with its unique challenges—processing and evaluating large sections of patient population means humongous volumes of data. Analysis of these overwhelming amounts of unstructured data is far more challenging than gathering data itself. That’s why healthcare organizations design new strategies to integrate digital technologies into their practices—for monitoring and analyzing patient data.
The Rise of Digital Healthcare
The rise of digital in healthcare has gained momentum over the last few decades. However, the shift to value-based healthcare has further increased the importance of digital and has made it an imperative rather than an option. Nevertheless, not every healthcare organization is chomping at the bit to adopt these changes.
Healthcare systems across the globe witness care providers’ attitude to new technologies as a major obstacle to digital technology adoption: physicians are hesitant towards digital adoption especially when it comes to payment models. However, the shift to value-based care models in today’s healthcare scenario highlights the fact that payments will be closely knitted to quality of care—increasing penalties for instances of healthcare reimbursements.
Care Coordination
Critical data aggregated through population health analytics facilitate better care coordination by providing deeper level of insights into patients’ behaviors and patterns—that optimize patient care and outcomes. This is specifically of higher significance to patients with chronic diseases and complex conditions that require more personalized and connected healthcare services—a behavior that could prevent their care providers from financial penalties.
Improving Patient Adherence and Reducing Readmissions
Another aspect of care coordination being tackled by PHM includes patient’s medication adherence and follow-up. This analyzes—obstacles to treatment and examines why patients are not adhering to medications or completing their treatments. With careful evaluation of these data, healthcare organizations can significantly reduce readmissions, improve adherence and quality of care.
Read more on: Proven Digital Strategies to Reduce Hospital Readmissions
What’s Ahead?
For years now, the concept of Population Health Management has been on the radar—but with emerging challenges and uncertainties in the healthcare ecosystem, it’s time that healthcare organizations adopted these solutions to drive population health outcomes. It is only going to get more complex: each year, more payments will be directly integrated to value-based care models, which signifies the rising need for deeper understanding of population health data.
Cost-effectiveness, a top priority for care providers, will eventually be linked to readmissions and the associated penalties. Therefore a key challenge will be: how can doctors treat patients with complex conditions with higher probability of readmissions—while preventing the financial consequences of hospital readmissions?
What’s the Answer?
Is it better patient management? Better patient data analysis and monitoring? New treatments? New medications? Or something else? If you have been considering the above questions, the answer is well—the combination of all these factors, well-orchestrated and integrated together to deliver over improved health outcomes.
Patient Management and follow-up will continue to be one of the top priorities, but since data needs to be analyzed longitudinally to measure its full impact, healthcare organizations need to have a broader perspective and devise long-term strategies to rise above the ongoing challenges presented by Population Health Management.
To learn more about Population Health Management strategies to drive up patient outcomes, talk to our team
From our humble beginnings as a healthcare start-up—to becoming a full-blown healthcare-exclusive digital transformation provider, our journey has been quite a remarkable one. Today, SolvEdge is a leading-edge Healthcare services and solutions provider—trusted by 450+ Hospitals, 3500+ Physicians and millions of patients across the globe.