T As the COVID-19 pandemic sweeps the world, it has illustrated cracks in the global healthcare ecosystem. As a result, there in a massive spike in demand for ambulatory, inpatient services and virtual health. The most critical areas likely to be impacted include the healthcare infrastructure, workforce and hospital equipment. From the infrastructure perspective, the U.S healthcare system is currently equipped with 46,000 ICU beds, operating at near full capacity on a regular basis.
Extensive measures like social-distancing and shelter-in-place are taken to mitigate the impact. However, the demand could still be at about 200,000 patients requiring ICU hospitalization, leading to potential demand—capacity gaps.
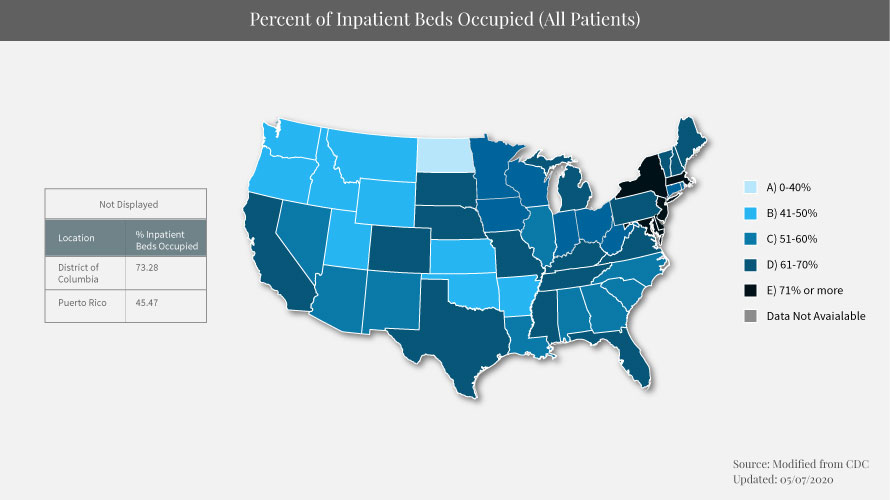
The Centers for Medicare and Medicaid Services (CMS) and the U.S Centers for Disease Control and Prevention (CDC) have shared their predictions on the potential surge in demand that is further expected to grow in the coming weeks. There is a shifting focus on flattening the curve — to address the hospital demand-capacity concern.
The Healthcare Capacity Management – Current Scenario
The healthcare capacity in the present scenario is static and cannot be exceeded. The federal government has taken several initiatives like patients over paperwork, Hospitals without walls to facilitate the temporary expansion of healthcare settings. However, besides infrastructure and equipment constraints, there is also a potential risk of a declining workforce – on the following scenarios.
- Frontline staff affected by COVID-19 and tested positive – who require to be quarantined. Nevertheless, telehealth platforms have come to rescue at this critical time of crisis—enabling quarantined physicians to offer virtual care
- Clinicians working around the clock – could lead to exhaustion and lower immune response— further increasing the chances of contracting the virus
- Healthcare professionals who stay back home to take care of their family members who might fall sick
- Protocols and operational measures that require healthcare workers to stay at inpatient facilities for several days post COVID-19 recovery - preventing them from getting back to care delivery
These factors may contribute to the declining health capacity from the workforce perspective.
Excess to Strained Capacity – Key Implications
The health capacity decline could mean deferred testing and care potentially increasing risks of incidents — that stem from undiagnosed and untreated individuals. This could be further influenced by supply-side shortage.
What is the role of virtual health?
Virtual health including telemedicine services and remote patient monitoring are the most secure ways to increase healthcare system capacity.
- Optimize Capacity—Virtual health helps leverage excess provider capacity from non-COVID-19 hotspot regions to maximize care
- Reduce In-person Visits—Facilitating social-distancing. It minimizes exposure and prevents the use of Personal Protective Equipment (PPE). ER doctors can leverage the platform to pay emergency room visits
- Maximize Workforce—Allows self-quarantined providers to continue to offer virtual support like tele-consultancy and e-visits
- Augment Scarce Intensive-care Physician Expertise—Intensive-care Physicians are a scarce workforce, and can be augmented through e-ICU solutions to get connected remotely. This helps extend the reach of intensivisit multifold
- Create New Capacity—Remote patient monitoring facilitates hospital-at-home-solutions enabling quick discharge of patients. This creates new capacity in-home and frees up inpatient capacity for new patients
The federal government has temporarily waived-off policies and eased restrictions in response to the COVID-19 pandemic. CMS has announced policies that augment the potential and reach of telemedicine services—like Medicare telehealth visits, virtual check-ins and e-visits Furthermore, the agency has relaxed the enforcement of HIPAA policies to harness the potential of virtual health visits through non-compliant telehealth platforms. The relaxation of these policies is key to the rising adoption of virtual health.
To learn more on the latest updates to telemedicine codes, click here