CMS’s Rule on Automating Prior
CMS’s Rule on Automating Prior Authorization: A Deep Dive

Blog
CMS’s Rule on Automating Prior Authorization: A Deep Dive

The new rule on the Prior Authorization process automation aims to eliminate the hassles of several mundane and manual administrative tasks, by automating and streamlining steps involved in Medical Billing Prior Authorization.
On 10th December 2020, the Centers for Medicare & Medicaid Services (CMS) has announced a new rule on the Prior Authorization process automation—to facilitate and improve data exchange between Care Providers and the Payers.
Healthcare data exchange between Payers and Providers has been a major administrative hurdle, hindering medical billing and impacting the efficiency of the healthcare revenue cycle management process. The new rule on the Prior Authorization process automation aims to eliminate the hassles of several mundane and manual administrative tasks, by automating and streamlining steps involved in Medical Billing Prior Authorization. The new rule requires Payers to develop new Application Programming Interfaces (APIs) to simplify and enhance data exchange, while maximizing patient care and boosting Patient Experiences (PX).
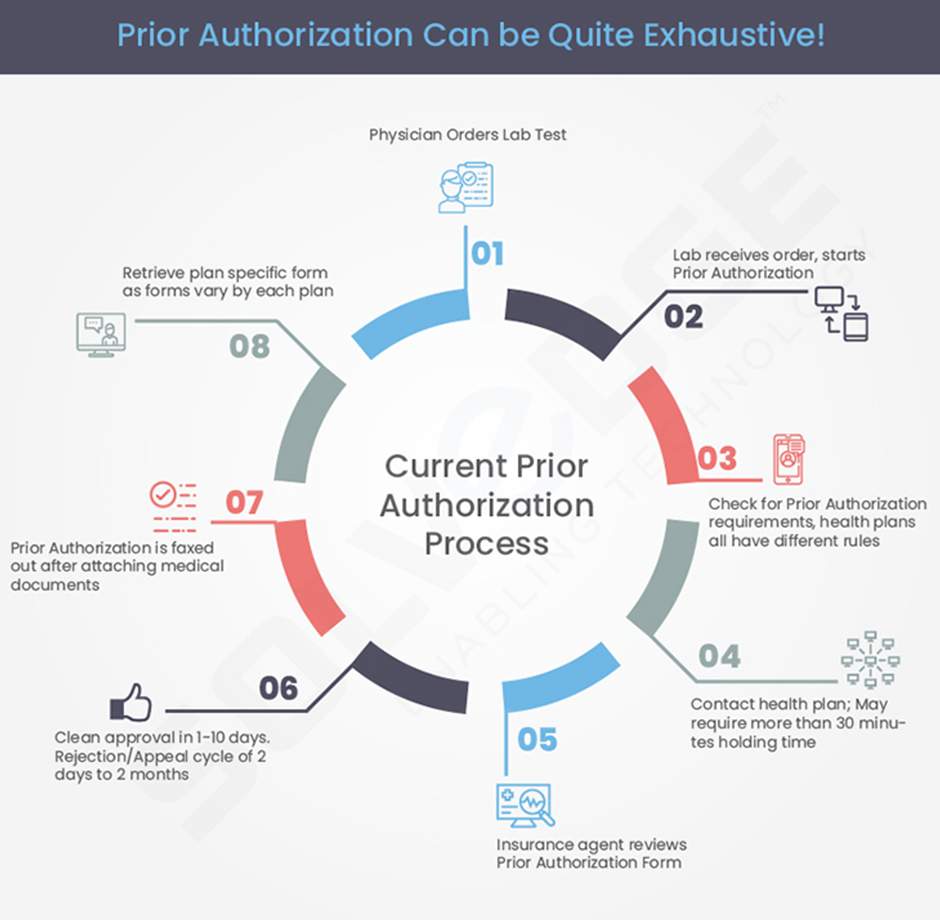
Providers have a common complaint that Prior Authorization has become quite an extensive task and consumes much of the hospital admins’ time with several complications involved in manual methods. This rule intends to reduce manual interventions, speed up the entire process, improve accuracies and drive efficiencies drastically.
The rule has a timeframe of 72-hours for Payers for emergency requests and seven calendar days for non-emergency requests. This is a huge time-saver for the care Providers and simplifies the Prior Authorization process at scale. The rule is applicable for all the major programs, including the Children’s Health Insurance Program, and other key health plans.
Prior Authorization is an additional burden on care Providers and causes Physician burnout to a great extent. Consider that a whopping 45% of Physicians submit their Prior authorization requests over the fax, while a staggering 59% are made over the phone.
Prior Authorization requires extensive processes where a hospital or a Practice needs to get approval from a Payer for a medical service or a medical supply. Even before a drug prescription, the Physician needs to obtainprior approval by submitting necessary documents to the Payer on the drug prescription. Moreover, the global health emergency has made it even more important to follow these policies in a more stringently manner.
The survey on Prior Authorization trends, conducted by the American Medical Association (AMA) to 1,000 Physicians revealed the following:
This proposed rule by CMS aims to streamline the Prior Authorization process by integrating FHIR-based APIs to seamlessly and securely exchange patient data. This enables patients to get a 360-degree view of their medical histories, while also facilitating data exchange between payers. It ensures that the key stakeholders of a patient’s journey including the Patients, Providers and the Payers are well-connected and well-equipped with the right information, at the right time.
While this proposed rule goes through the processes before implementation, you can explore more on Prior Authorization services from an established healthcare revenue cycle management company like SolvEdge.
From our humble beginnings as a healthcare start-up—to becoming a full-blown healthcare-exclusive technology solutions provider, our journey has been quite a remarkable one. Today, SolvEdge is a leading-edge Healthcare services and solutions provider—trusted by 450+ Hospitals, 3500+ Physicians and millions of patients across the globe. The SolvEdge healthcare framework is revolutionary because our approach is based on an absolute dedication to insight-driven analytics on financial outcomes and expenses. Hundreds of healthcare organizations have saved millions of dollars working with SolvEdge digital healthcare technology solutions in identifying and reducing costs effectively. To learn more about our Prior authorization and other medical billing services, talk to our team.
From our humble beginnings as a healthcare start-up—to becoming a full-blown healthcare-exclusive digital transformation provider, our journey has been quite a remarkable one. Today, SolvEdge is a leading-edge Healthcare services and solutions provider—trusted by 450+ Hospitals, 3500+ Physicians and millions of patients across the globe.