5 Key Strategies to Effectively
5 Key Strategies to Effectively Streamline and Overcome Prior Authorization Burdens

Blog
5 Key Strategies to Effectively Streamline and Overcome Prior Authorization Burdens

Demystifying and streamlining the pre-authorization process could be a game-changing factor in healthcare—significantly transforming patient care and the overall patient outcomes.
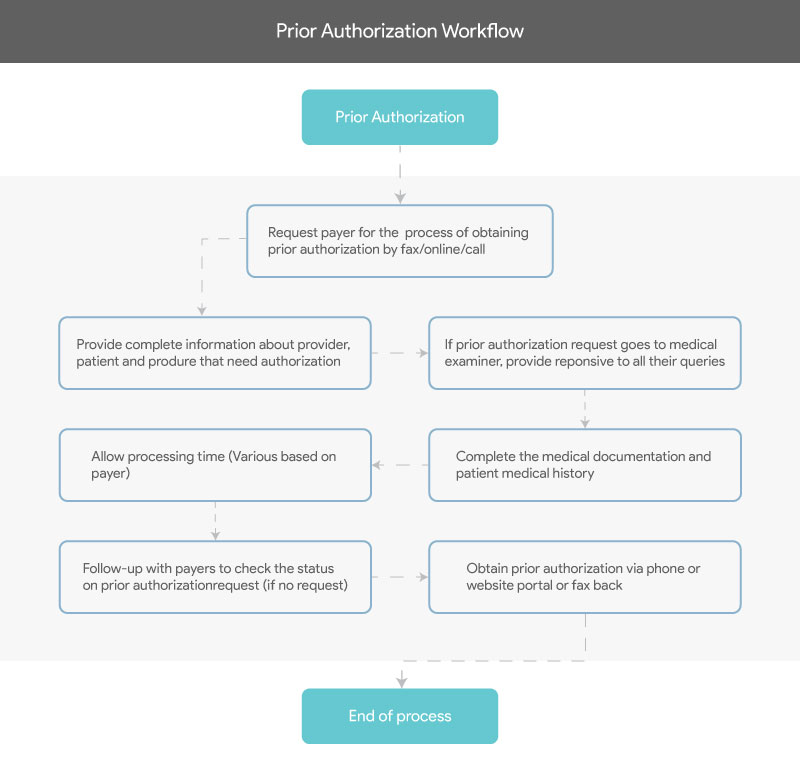
Prior authorization is an essential process in medical billing as also the compelling need for care providers to get prior authorizations from payers before offering any care service could be one of the greatest hindrances to providing quality care.
Consider that organizations are still following manual processes for request submissions and are collecting information through fax or phone. Also, the complexities involved in prior authorizations, such as a knee replacement surgery in most cases, need approvals for each item or service like the device, crutches, pre-op and post-op visits, etc., instead of getting them approved in one go.
It takes an extensive amount of the care provider’s time and efforts to furnish all the relevant documentation to the insurance companies. Research among Hospitals and Physicians indicate that Prior authorization was reported as the No.1 complaint—severely impacting patient care.
Here’s the good news. The prior authorization process need not be complicated and could be simplified to a great extent. Research reveals that about 90 percent of prior authorizations are approved by the insurers. However, it goes through stringent processes of exhaustive paperwork as well as multiple interactions and explanations.
Demystifying and streamlining the pre-authorization process could be a game-changing factor in healthcare—significantly transforming patient care and the overall patient outcomes.
A recent study by the Journal of the American Medical Association (JAMA) network indicates that administrative burdens alone cost the healthcare industry a staggering $266 billion a year and is prognosticated to grow further. This shows that we have much work to do. Here are five key strategies that will help you successfully rise above the prior authorization challenges.
Care providers who are well-informed and adhere to the payer’s specific requirements needn’t have to get prior authorizations. Physicians are reported to spend a whopping 15 hours every week on prior authorizations, and even cutting this in half the time could make a huge difference—helping you spend more quality time on higher priority tasks.
Automation is one of the key strategies that can simplify and improve the accuracies of the pre-authorization process by quickly identifying the most suitable treatment or medication. Say, a care provider wants to order an MRI, automation technologies can leverage real-time analytics to suggest if it was warranted instantly. . A Council for Affordable Quality Healthcare (CAQH) report indicates that just 12 percent of prior authorization requests are made electronically against 100 percent of claims submitted electronically. Adopting automation solutions would drastically eliminate time-consuming and tedious manual processes to reduce hospitals and care practices costs.
Clear and transparent communication between providers and payers on the guidelines on medication/services that need prior authorization and the supporting documents required—would help streamline the overall process. To support this drive, the Centers for Medicare & Medicaid Services (CMS) has announced an initiative that allows providers interact with the payer platform through a secure environment to instantly identify whether or not a specific process needs prior authorization and the relevant documents required for the operation.
When a patient changes their health insurance provider, a whole new process and repeated protocols are usually required before treatment, which could tremendously impact the patient’s health condition and additional treatment costs for the Physician. Establishing a streamlined approach to accepting previous insurer’s prior authorization could go a long way in delivering timely care to the patients—while driving down unnecessary costs.
Manual methods and legacy systems could drastically slow down the pre-authorization process—negatively impacting patient care and outcomes. An American Medical Association (AMA) report shows that about 65 percent of Physicians reported at least one day of the delay in prior authorization process and 27 percent of them reported a delay of three days or more. This delay often causes patients to abandon treatments, which can be prevented by leveraging automation solutions to speed up approvals.
To learn more about how SolvEdge can help your healthcare organization accelerate the prior Authorization process, talk to our team.
From our humble beginnings as a healthcare start-up—to becoming a full-blown healthcare-exclusive digital transformation provider, our journey has been quite a remarkable one. Today, SolvEdge is a leading-edge Healthcare services and solutions provider—trusted by 450+ Hospitals, 3500+ Physicians and millions of patients across the globe.